| Now that you have been diagnosed with a kidney stone should you change your diet? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Patients who have had kidney stones often ask if they need to change their diet in order to prevent future
recurrence. If you are diagnosed with a kidney stone for the first time, you
have a 60% lifetime chance of forming another stone. While most stones pass
spontaneously, some require surgical intervention. However, non-surgical methods
are necessary to reduce the risk of future recurrence.
Sometimes doctors do
special blood and urine tests to find out the underlying cause of stone
formation. Based on these tests, your doctor may prescribe medications or make
dietary recommendations. 30% of the time no definite cause can be identified.
Long-term medical therapy has potential side effects often forcing patients to
stop the medicines. Random dietary changes based on advice given by friends or
relatives may be counter-productive. The following are general dietary
recommendations for all stone formers regardless of the type of their stone.
Fluids This is probably the most important of all dietary changes that may influence your stone recurrence. Low fluid intake makes urine more concentrated and more acidic both of which may promote stone formation. High fluid intake has been shown to reduce the risk of stone formation in several ways. The amount of fluid you drink should be enough for you to produce 2 liters of urine per day. You may need to drink more water in the summer than winter. The kind offluid is not so important, although it is better to drink non-dairy and low sodium fluids (e.g. Gatorade and some sodas are high in sodium.) Water is best and a good starting point is 6 to 8 full 8 oz. glasses per day. Calcium Most people think that if they have had a kidney stone, they need to cut back on their calcium intake. A low calcium diet may actually increase the risk of stone formation in some patients. It has been shown that men on a high calcium diet have 34% less risk of stone formation. Only few patients with calcium stones will benefit from a low calcium diet. You need to be tested to find out if you are among those. Some patients may need to increase their calcium intake in order to reduce their risk of stone formation. Postmenopausal women who are on calcium supplements have no increased risk of stone formation. Sodium A high salt diet increases the amount of calcium ill the urine. This effect is more pronounced in stone patients who have high calcium in their urine ( not all stone formers have high urinary calcium.) It's recommended that all stone formers cut back on the amount of their salt intake. Protein Incidence of kidney stones is higher in people on a high protein diet. Vegetarians have a much lower incidence of stone disease. A high protein diet increases urinary calcium, oxalate, uric acid, urine acidity and reduces the urinary citrate .. All of these factors increase the risk of stone formation. All stone formers are recommended to reduce the amount of their animal protein intake. Of note, the amount of carbohydrate and fat in your diet does not influence stone formation. Oxalate A few patients with calcium oxalate stones may have high oxalate in their urine and may need to reduce the amount of their dietary oxalate. See table below for a brieflist of high oxalate foods A list of high oxalate foods
Alcohol There is no association between alcohol consumption and stone risk. Chronic alcohol use increases the amount of calcium and uric acid in the urine but these patients are at no higher risk of stone formation. It's thought that the increased urine production associated with alcohol use may be beneficial prevention of stones. Citrate Citrate is a naturally occurring substance in the urine that prevents stone formation. The amount of urinary citrate can be measured in a 24 hour urine collection. If this is found to be low, you will need to take a regular daily medication. The amount of citrates in fruit is not high enough to raise urinary citrate unless large amounts are taken everyday. In some patients with only moderate reduction of citrate in urine drinking four glasses of lemonade everyday may be enough to restore the citrate levels to normal. 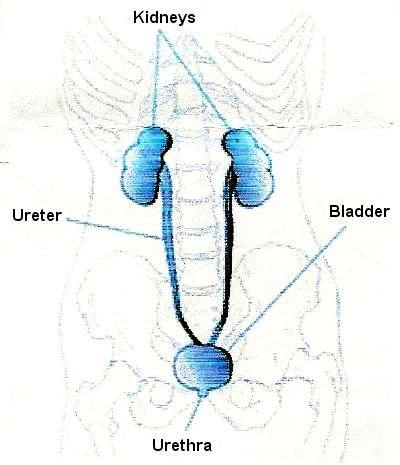 Conclusion Conclusion
All stone formers need to cut back on the amount of animal protein and salt in their diet and increase their fluid intake. No change in calcium, oxalate, and citrate is necessary unless you are tested and found to have a specific problem Most stone formers do not need to be tested for these specific problems. Recurrent stone formers or those at high risk of recurrence are usually tested. Kidney stones What are kidney stones? When certain substances in the urine become concentrated, they crystallize to form rock like objects called stones. The vast majority of stones are formed in the kidney and are calcium based (most common of which is calcium oxalate.) The stones may stay in the kidneys and grow or they may get dislodged and pass down the ureter into the bladder. If a stone gets lodged in the ureter urine backs up and stretches out the kidney like a water balloon. The condition is called hydronephrosis What causes kidney stones? There are many factors that contribute to kidney stone formation. The most common of which is the lack of hydration. If a person is prone to stone formation and becomes dehydrated, his or her urine would be less dilute and the concentrated substances would be more likely to crystallize into stones. Many other factors like diet, anatomy of the urinary system and metabolism may be involved. A strong family history of stone formation also increases the risk of stone development. What are the symptoms? A stone in the kidney mayor may not cause pain. Pain from kidney stones result from blockage of urine flow and subsequent swelling of the kidneys. The pain is usually located in the flank ( the part of the back just under the rib cage) but may be felt in the groin when getting close to the bladder. The pain usually comes suddenly and can make the person feel nauseated. The pain can also come and go over a period of time. Some patients may pass blood in the urine. It's very difficult to predict which stones will cause minor symptoms and which ones will cause severe symptoms. Treatment options! The vast majority of stones will pass spontaneously. All smaller stones should be given a trial of passage if the symptoms can be controlled with oral pain medications. Stone passage depends on the size and location of the stone ( See Tables 1 and 2.) In general the smaller the stone and further down the ureter, the more likely it'll pass with observation. It may take as little as 1-2 days or up to 4-5 weeks to pass a stone. It's very difficult to predict how long it'll take to pass a stone. Table 1
Table 2
There are many options available if a stone doesn't pass. The choice of treatment modality is based on stone size and location. Your-urologist can guide you in that respect. l. ESWL ( Extracorporeal Shock Wave Lithotripsy) This is a method where patients receive shock waves (non-electrical ) through a water medium into the body and directed to the stone. The stone is fragmented into many pieces with minimal injury to the body. The pieces of stones are subsequently passed in the urine. There is no way to predict on how good or bad stones fragment. The procedure is usually performed under general anesthesia and is done mainly for stones in the kidney and upper ureter. 2. Ureteroscopy. This procedure is also done under anesthesia and involves passing a scope into the bladder and up into the narrow ureter. It is usually performed for stones in the lower ureter. The stones can be either broken up into pieces by a laser or removed with a basket-like gadget. A stent ( a temporary plastic tube) is usually placed after the procedure. 3. PCNL (Percutaneous Nephrolithotomy). This method is also done under general anesthesia and involves placing a scope directly through the skin of your back and into the kidney. The stones are fragmented through the scope by using ultrasound and fragments sucked out. After the procedure a kidney tube is placed temporarily through the skin and the patient usually stays in the hospital for 1-2 days. This is the most.invasive .of, all treatment modalities and is generally reserved for larger stones. Здоровье www.pseudology.org |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||